Syringe Exchange Starts a Conversation
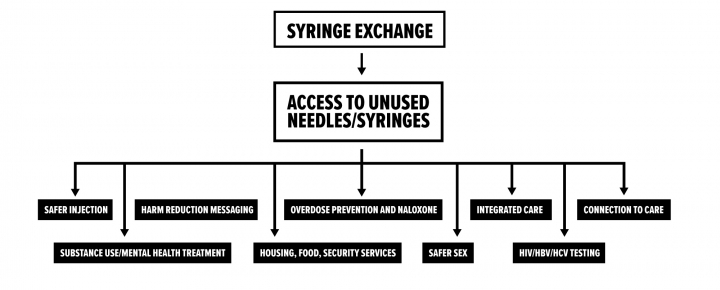
Syringe service programs (SSPs), are also known as syringe exchange programs (SEPs) or needle exchange programs (NEPs). They are community-based programs that provide access to sterile needles and syringes free of cost and facilitate safe disposal of used needles and syringes.
SSPs are an effective component of a comprehensive, integrated approach to HIV and hepatitis prevention among people who inject drugs.
Most SSPs offer other services, such as overdose prevention; referral to substance use disorder treatment programs (including medication-assisted treatment), and counseling and testing for HIV and hepatitis C.
SSPs have expanded rapidly across the U.S. in recent years and play a key role in responding to the national opioid crisis. States have legalized syringe exchange and organized their programs using varied strategies and pathways.
Syringe service programs are often the first encounter that people who inject drugs have with health and social services. These programs provide a resource for PWID to seek out additional services, and the referrals to treatment services made by SSPs often come at the request of program participants. In the first seven months of operation of the New Haven syringe exchange program, 25% of participants requested drug treatment referrals. 60% of those individuals subsequently entered a detoxification program (10). Of the 40% who did not enter treatment, lack of health insurance was cited as the reason.
Florida has one legal syringe exchange that serves Miami-Dade county (legalized in 2015), and has seen how costly it can be to have no syringe exchange program. In a study of people who inject drugs (PWID) before syringe exchange programs were implemented, over the course of one year 349 PWID were admitted to a county safety net hospital with bacterial infections from drug injection (preventable by use of sterile syringes). These hospitalizations resulted in $11.4 million in healthcare expenses and 17 deaths. The vast majority of hospitalized PWID (92%) were either uninsured or relied on publicly funded insurers such as county, state and federal programs. While it is customary for hospitals to bill in excess of expected payment for services rendered based on pre-negotiated reimbursement rates, Florida Medicaid was billed $18.4 million over the study period for injection drug use-related infections (4).
Hawai’i established syringe exchange programs in 1989, and became the first state to fully fund and coordinate syringe exchange programs through its department of public health. Hawai’i’s success and efficacy can be seen through its reduction of the transmission of HIV. In the U.S., one third of all HIV infection cases are due to injection drug use. In Hawai’i this proportion is only 13%. Further, among syringe exchange participants in Hawai’i, there is an HIV prevalence of 0% (12).
Indiana has no comprehensive, statewide syringe exchange program, and until 2015 did not have legal syringe exchange. In Scott County, IN, a rural community in the southern portion of the state, there were five cases of HIV diagnosed from 2004 – 2014. During this time, opioid use and injection drug use began to increase in Scott county. Then, from November 2014 – August 2015, 181 residents tested positive for HIV. After declaring a state of emergency in March 2015, Governor Mike Pence issued an executive order legalizing syringe exchange. The program began operation in August 2015. Between September and October 2015, not a single person tested positive. Indiana will continue to incur costs from this outbreak for decades: the lifetime treatment cost for one person with HIV infection is $378,668. Other states, like New York, Wisconsin, and Hawai’i have effectively eliminated HIV through their syringe exchange programs and avoided such human and financial costs (5).
No study has ever found that syringe exchange programs increase drug use or rates of crime. A Maryland study examined crime rates and arrest data in a neighborhood during the six months before and after the opening of a syringe exchange program. The study found that when controlling for all variables, the number of arrests decreased in the period following the opening of the syringe exchange (8).
Syringe exchange programs have a long history of facilitating entry into treatment programs for substance use disorders. A 2006 study of 1,490 people who injected drugs in a Maryland community explored whether or not people sought out treatment services through their syringe exchange programs. Between 1994 and 1998 when the first syringe exchange opened in the community, 25% of the program participants entered detoxification. The study found that needle exchange program participants were 3.2 times more likely to enter detoxification than people in the community who used drugs but did not participate in the needle exchange program (9).
For those persons who do not participate in a syringe exchange program, the process of entering treatment can be daunting – long wait times, lack of transportation, and insurance paperwork can make navigating the treatment system extremely difficult to an individual. Although syringe exchange is not legal in Missouri, a syringe exchange program still operates. In this program, employees keep files on each syringe exchange program participant. During each visit to the syringe exchange, employees discuss readiness to enter treatment and make notes of participants’ readiness. Once the individual is ready to enter a treatment program, the employee navigates and arranges entrance into the treatment program. Because syringe exchange programs have relationships with drug treatment programs, this linkage to care is easily navigated (11).
In 2006, New Jersey legalized a syringe exchange pilot program. Through 2011, the syringe access program enrolled 9,912 participants. 22% of those participants (2,160) were admitted to methadone or suboxone treatment programs. Just under 2 million syringes were distributed, and the state elected to continue the program (6).
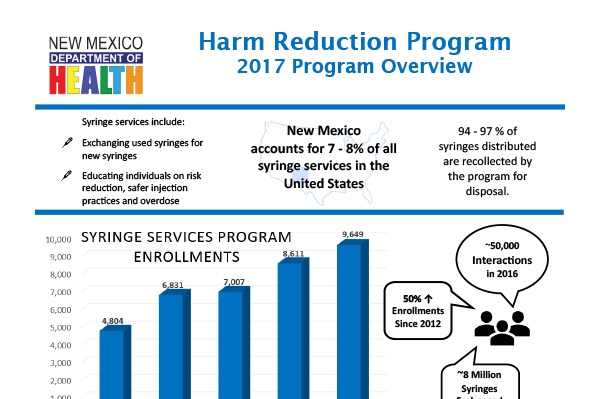
New Mexico’s department of public health administers the state’s syringe service program. There are 40 syringe exchange programs in the state, and most are operated within local public health departments. 9 are operated by community-based organizations. Syringe exchange became legal in 1997, and now the program has 40,000 participants per year and exchanges 4 million needles per year. The syringe service programs offer naloxone and overdose prevention services, provide testing for HIV and hepatitis, offer counselling and support groups, and provide suboxone treatment.
Syringe exchange programs are often believed to encourage and promote drug use. However, in a study of syringe exchange participants in New York, new participants decreased their injection frequency by eight percent after enrolling in a syringe exchange program (14).
Syringe exchange programs began to operate in New York in 1988. In 1990, 54% of injecting drug users were HIV positive, and 90% had hepatitis C. By 2012, 3% were HIV positive, and 63% had hepatitis C, illustrating the power of syringe exchange programs to significantly reduce infectious disease prevalence in a population. During this period, the syringe exchange programs grew from exchanging 250,000 syringes annually to exchanging over 3 million annually (14).
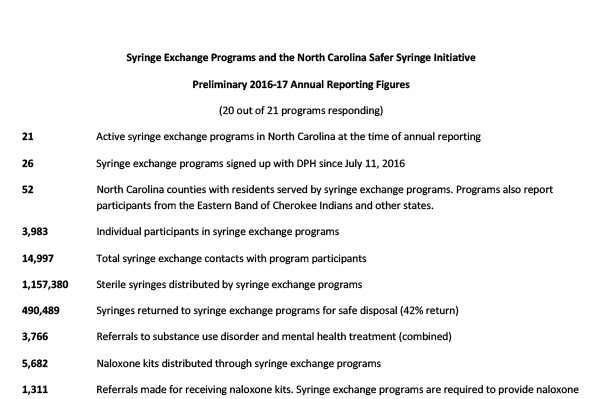
North Carolina legalized syringe exchange programs in 2015. Since then, the state has developed 21 programs that serve 52 counties. Since legalization, 3,983 individuals have participated in syringe exchange programs, resulting in a total of 14,997 contacts with program participants and 1,157,380 sterile syringes distributed.
Syringe exchange programs serve as excellent opportunities to distribute naloxone, and to make connections to treatment programs – NC has made 3,766 referrals to substance use disorder treatment and distributed 5,682 naloxone kits. Program participants have reported 2,187 overdose reversals.
These programs have administered 738 hepatitis C tests, identified 138 positive hepatitis C results, and administered 2,647 HIV tests, with 6 positive results.
Utah legalized syringe exchange programs in May 2016. The law required the Utah Department of Health to enroll agencies to run syringe exchange programs, collect data, and make reports to the state legislature on the programs. The syringe exchange programs are required to provide new syringes, offer syringe disposal, and make referrals or offer services for HIV/HCV testing, substance use disorder treatment, and naloxone and overdose prevention. The law did not provide funding for the programs. Since the launch of the programs in December 2016, Utah has distributed over 180,000 syringes, collected almost 70,000 used syringes, and worked with over 5,000 participants. The program is new, and program evaluation takes time and money – it will take several years to learn how the program impacts rates of infectious disease and how successfully programs connect Utah residents into services (3).
Since 1995, the AIDS Resource Center of Wisconsin and the Wisconsin state department of public health have operated 10 syringe exchange programs throughout the state. In 1995, there were 235 new HIV infections among people who inject drugs. However, in 2015, there were two new HIV infections in this community (1).
In 2015, of 47,680 syringe exchange participants, 8,046 referrals to drug treatment were made (1).
Syringe exchange programs often make referrals to treatment. A study of one syringe exchange program found that over the course of one week, 40% of participants entered treatment when offered services by a case manager or social worker. Among these participants, the case manager arranged payment, transportation, and enrollment in a treatment program. Among participants who were handed a paper referral but did not receive assistance from a case manager, 26% entered a treatment program within the week (2). Both case management services and referrals from syringe exchange programs are useful pathways to link people into treatment services.
A 2000 study of syringe exchange participants in Seattle found that people who participated in a syringe exchange were 2.5 times more likely to reduce their injection frequency than people who had never participated in a syringe exchange program. They were 3.5 times more likely to stop injecting drugs all together (compared to those who had never participated in a syringe exchange program). New users of syringe exchange programs were five times more likely to enter drug treatment programs than those who did not use the programs (13).
Washington state legalized syringe exchange in 1992. Their state health department coordinates the work of many different programs spread around the state. In 2016 87,806 individuals were served, the majority through mobile syringe exchange programs, non-traditional community locations, deliveries, outreach, clinics, and community-based organizations.
In 2016, 16,719,311 sterile syringes were distributed. 5,294 people were referred to drug treatment were made, as were 8,376 health care referrals, and 11,401 people participated in syringe exchange.
Syringe exchange programs are also an excellent opportunity to distribute naloxone and are an extremely effective pathway to prevent overdose deaths. In WA, 2,728 naloxone kits were distributed in the first eight months of 2017. 1,814 people received kits, including 349 law enforcement officers and 1,465 people who use drugs. In just eight months, 392 overdose reversals were reported. 100% of reversals were performed by drug users.
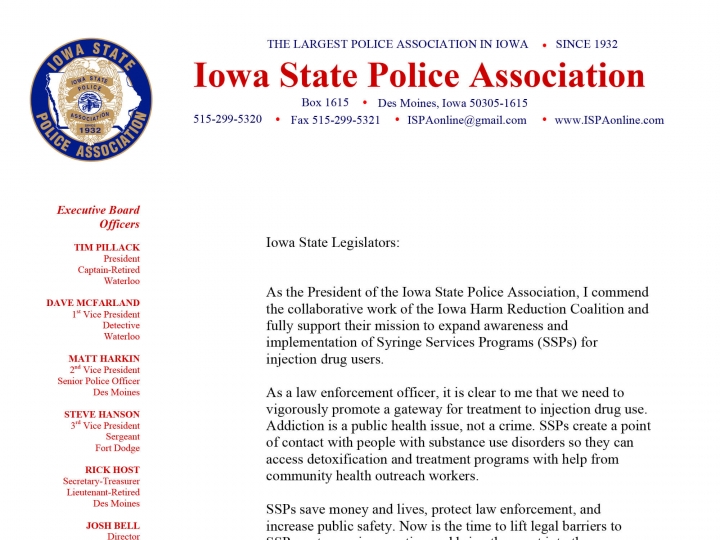
Law Enforcement Officers Support Syringe Service Programs and Needle Exchange

Chief Michael Tupper
Marshalltown
Chief of Police, Marshalltown Police Department
“SSPs save money, lives, and take used needles off the streets, which protects both law enforcement and the public. Now is the time to lift legal barriers to SSPs, get more in operation, and bring them out into the open through political support.”

Chief Mark Prosser
Storm Lake
Storm Lake Police Department
“I fully support the implementation of Syringe Services Programs (SSPs) for injection drug users. Recognizing the increase in heroin related incidents and deaths, it is important that law enforcement develop partnerships with a variety of stakeholders to have a an effective response to its use. Many police chiefs understand that while heroin use is a legal problem, it is primarily a public health problem that should be handled with combined efforts with public health officials. The challenge is how to get those who need treatment into the appropriate programs.”

Senator Dan Dawson
Council Bluffs
Iowa Senate District 8
Special Agent
Iowa Division of Criminal Investigation
“One of the first things I thought was, needle exchange, what the heck? As a law enforcement officer, its something that I initially had an adverse reaction to. But when I started doing some more reading and we started having conversations, my mind was changed by just looking at the data.”
“[Among Republican legislators] I think the support, you’d be shocked to know how much support there really is when we start talking behind the scenes. Like anything else we deal with in the legislature, you have the moral implications vs. the costs, and the cost savings. And those are the three tiers we look at when we have these discussions. When we drill down into the data that is out there, the data clearly shows that the majority of hepatitis and AIDS infections comes from dirty needles. This program has been shown to be effective in other parts of the United States to reduce diseases. Most persons, when you show them the data, its just a matter of having thoughtful conversations and breaking it down. There is a lot of merit to this reducing infectious diseases. The most convincing case I will make, is that the data clearly shows that a syringe exchange program does lower the hepatitis C and HIV transmission rates. If there is a concern about individuals using money for needles instead of textbooks, you’re going to save money for textbooks and education down the road because we are going to lower health care costs inside our prison system.”

Chief Jody Matherly
Iowa City
Iowa City Police Department
“Recognizing the increase in heroin related incidents and deaths, it is important that law enforcement develop partnerships with a variety of stakeholders to have an effective response to its use. Many police chiefs understand that while heroin use is a legal problem, it is primarily a public health problem that should be handled by public health officials. The challenge is how to get those who need treatment into the appropriate programs. SSPs create a point of contact with people with substance use disorders so they can access detoxification and treatment programs with help from community health outreach workers.”

Senator Kevin Kinney
Oxford
Iowa Senate District 39
Lieutenant (retired)
Johnson County Sheriff’s Office
“The opioid addiction crisis affects Iowans from all walks of life every day, and it’s creating another epidemic: sharing needles to inject the drug. As a result, Hepatitis C and HIV are on the rise in Iowa. To help stem the tide, advocates recommend syringe exchange programs that provide clean needles to those struggling with addition. The Iowa Department of Public Health and the Iowa Harm Reduction Coalition promote these programs to limit the impact of the opioid crisis. SF 2294 would allow syringe services programs in Iowa, under the oversight of the Department of Public Health. Although some believe this proposal would enable addicts, similar programs in other states have successfully reduced outbreaks of Hepatitis C and HIV, and have helped many get the substance abuse treatment they need. Some estimates show needle exchange programs make it five times more likely an addict will seek treatment.”

Representative Wes Breckenridge
Newton
Iowa House District #29
Lieutenant (retired)
Newton Police Department
“As a retired police officer, I see the value of a needle exchange program. Statistics support that it does NOT increase drug use. Needle exchanges would increase police officer and community safety. Ready availability of clean needles and cleaner disposal of dirty ones would greatly decrease accidental exposure to needles by police and the public. Studies confirm needle exchanges reduce disease transmission and increase substance abuse treatment, both of which increase public safety.”
Letters of support from law enforcement
Law Enforcement & Syringe Exchange Programs: The North Carolina Experience.
David’s story
SSPs create opportunities for healing
David is a 42 year old Cedar Rapids resident who is the manager of a local restaurant. He and his wife have used heroin and methamphetamine together for many years. In the fall of 2017, David decided he wanted to stop using heroin and meth, but wanted to “wean himself off,” rather than beginning a suboxone or methadone program. Each week he would report to IHRC that he had reduced his daily dosing incrementally, and he used a number of strategies to use increasingly less – he even added weight to his scale so he would not know how much less he was using. He compared it to what someone might do if they were trying to lose weight using diet and exercise. Then one day, he decided he was ready to taper completely. The first day he quit was hard – so an IHRC outreach worker spent three hours with him, providing support and counselling. Pursuing sobriety wasn’t easy – each day, outreach workers checked in with him to offer affirmation and encouragement in support of his choices. For David, the transition from actively using to reducing his use to becoming abstinent was smoothly supported through trusting relationships established through his harm reduction program.

Ben’s Story
SSPs offer connections to treatment
Ben is a 26 year old from Iowa City who has been using heroin for several years. In the fall of 2017, he met the Iowa Harm Reduction Coalition (IHRC) while they were conducting community outreach. He received a naloxone kit and was grateful for the assistance, but was disappointed not to be able to receive syringes – he worried about contracting HIV or hepatitis from the friends he regularly used with. After meeting IHRC, he returned often to receive naloxone and spend time with some of the outreach workers he had formed friendships with. Several months later, Ben returned to IHRC to tell the outreach workers that he was quitting – he was sick of using and wanted to enroll in a suboxone program. But he was having difficulty finding a provider or a clinic – the wait time for one clinic was nine weeks; another required that he find a ride to Cedar Rapids each day for methadone; another required he pay out of pocket; some required he have a valid government ID. When he told IHRC’s outreach workers about the difficulty he was experiencing, they were able to offer him assistance. But it wasn’t easy – it took hours spent on the phone, looking for treatment providers who had space available to take on a new patient. Finally, through a physician that the IHRC outreach workers had an existing relationship with, IHRC was able to find a place in a suboxone treatment program that worked for Ben’s needs. Across the country, harm reduction programs offer a point of connection to people who use drugs, and create supportive relationships like these. These programs do much more than just offer a piece of paper as a referral.
SSPs around the United States
Syringe service programs are often the first encounter that people who inject drugs have with health and social services. These programs provide a resource for PWID to seek out additional services, and the referrals to treatment services made by SSPs often come at the request of program participants. In the first seven months of operation of the New Haven syringe exchange program, 25% of participants requested drug treatment referrals. 60% of those individuals subsequently entered a detoxification program (10). Of the 40% who did not enter treatment, lack of health insurance was cited as the reason.
Florida has one legal syringe exchange that serves Miami-Dade county (legalized in 2015), and has seen how costly it can be to have no syringe exchange program. In a study of people who inject drugs (PWID) before syringe exchange programs were implemented, over the course of one year 349 PWID were admitted to a county safety net hospital with bacterial infections from drug injection (preventable by use of sterile syringes). These hospitalizations resulted in $11.4 million in healthcare expenses and 17 deaths. The vast majority of hospitalized PWID (92%) were either uninsured or relied on publicly funded insurers such as county, state and federal programs. While it is customary for hospitals to bill in excess of expected payment for services rendered based on pre-negotiated reimbursement rates, Florida Medicaid was billed $18.4 million over the study period for injection drug use-related infections (4).
Hawai’i established syringe exchange programs in 1989, and became the first state to fully fund and coordinate syringe exchange programs through its department of public health. Hawai’i’s success and efficacy can be seen through its reduction of the transmission of HIV. In the U.S., one third of all HIV infection cases are due to injection drug use. In Hawai’i this proportion is only 13%. Further, among syringe exchange participants in Hawai’i, there is an HIV prevalence of 0% (12).
Indiana has no comprehensive, statewide syringe exchange program, and until 2015 did not have legal syringe exchange. In Scott County, IN, a rural community in the southern portion of the state, there were five cases of HIV diagnosed from 2004 – 2014. During this time, opioid use and injection drug use began to increase in Scott county. Then, from November 2014 – August 2015, 181 residents tested positive for HIV. After declaring a state of emergency in March 2015, Governor Mike Pence issued an executive order legalizing syringe exchange. The program began operation in August 2015. Between September and October 2015, not a single person tested positive. Indiana will continue to incur costs from this outbreak for decades: the lifetime treatment cost for one person with HIV infection is $378,668. Other states, like New York, Wisconsin, and Hawai’i have effectively eliminated HIV through their syringe exchange programs and avoided such human and financial costs (5).
No study has ever found that syringe exchange programs increase drug use or rates of crime. A Maryland study examined crime rates and arrest data in a neighborhood during the six months before and after the opening of a syringe exchange program. The study found that when controlling for all variables, the number of arrests decreased in the period following the opening of the syringe exchange (8).
Syringe exchange programs have a long history of facilitating entry into treatment programs for substance use disorders. A 2006 study of 1,490 people who injected drugs in a Maryland community explored whether or not people sought out treatment services through their syringe exchange programs. Between 1994 and 1998 when the first syringe exchange opened in the community, 25% of the program participants entered detoxification. The study found that needle exchange program participants were 3.2 times more likely to enter detoxification than people in the community who used drugs but did not participate in the needle exchange program (9).
For those persons who do not participate in a syringe exchange program, the process of entering treatment can be daunting – long wait times, lack of transportation, and insurance paperwork can make navigating the treatment system extremely difficult to an individual. Although syringe exchange is not legal in Missouri, a syringe exchange program still operates. In this program, employees keep files on each syringe exchange program participant. During each visit to the syringe exchange, employees discuss readiness to enter treatment and make notes of participants’ readiness. Once the individual is ready to enter a treatment program, the employee navigates and arranges entrance into the treatment program. Because syringe exchange programs have relationships with drug treatment programs, this linkage to care is easily navigated (11).
In 2006, New Jersey legalized a syringe exchange pilot program. Through 2011, the syringe access program enrolled 9,912 participants. 22% of those participants (2,160) were admitted to methadone or suboxone treatment programs. Just under 2 million syringes were distributed, and the state elected to continue the program (6).
New Mexico’s department of public health administers the state’s syringe service program. There are 40 syringe exchange programs in the state, and most are operated within local public health departments. 9 are operated by community-based organizations. Syringe exchange became legal in 1997, and now the program has 40,000 participants per year and exchanges 4 million needles per year. The syringe service programs offer naloxone and overdose prevention services, provide testing for HIV and hepatitis, offer counselling and support groups, and provide suboxone treatment.
Syringe exchange programs are often believed to encourage and promote drug use. However, in a study of syringe exchange participants in New York, new participants decreased their injection frequency by eight percent after enrolling in a syringe exchange program (14).
Syringe exchange programs began to operate in New York in 1988. In 1990, 54% of injecting drug users were HIV positive, and 90% had hepatitis C. By 2012, 3% were HIV positive, and 63% had hepatitis C, illustrating the power of syringe exchange programs to significantly reduce infectious disease prevalence in a population. During this period, the syringe exchange programs grew from exchanging 250,000 syringes annually to exchanging over 3 million annually (14).
North Carolina legalized syringe exchange programs in 2015. Since then, the state has developed 21 programs that serve 52 counties. Since legalization, 3,983 individuals have participated in syringe exchange programs, resulting in a total of 14,997 contacts with program participants and 1,157,380 sterile syringes distributed.
Syringe exchange programs serve as excellent opportunities to distribute naloxone, and to make connections to treatment programs – NC has made 3,766 referrals to substance use disorder treatment and distributed 5,682 naloxone kits. Program participants have reported 2,187 overdose reversals.
These programs have administered 738 hepatitis C tests, identified 138 positive hepatitis C results, and administered 2,647 HIV tests, with 6 positive results.
Utah legalized syringe exchange programs in May 2016. The law required the Utah Department of Health to enroll agencies to run syringe exchange programs, collect data, and make reports to the state legislature on the programs. The syringe exchange programs are required to provide new syringes, offer syringe disposal, and make referrals or offer services for HIV/HCV testing, substance use disorder treatment, and naloxone and overdose prevention. The law did not provide funding for the programs. Since the launch of the programs in December 2016, Utah has distributed over 180,000 syringes, collected almost 70,000 used syringes, and worked with over 5,000 participants. The program is new, and program evaluation takes time and money – it will take several years to learn how the program impacts rates of infectious disease and how successfully programs connect Utah residents into services (3).
Since 1995, the AIDS Resource Center of Wisconsin and the Wisconsin state department of public health have operated 10 syringe exchange programs throughout the state. In 1995, there were 235 new HIV infections among people who inject drugs. However, in 2015, there were two new HIV infections in this community (1).
In 2015, of 47,680 syringe exchange participants, 8,046 referrals to drug treatment were made (1).
Syringe exchange programs often make referrals to treatment. A study of one syringe exchange program found that over the course of one week, 40% of participants entered treatment when offered services by a case manager or social worker. Among these participants, the case manager arranged payment, transportation, and enrollment in a treatment program. Among participants who were handed a paper referral but did not receive assistance from a case manager, 26% entered a treatment program within the week (2). Both case management services and referrals from syringe exchange programs are useful pathways to link people into treatment services.
A 2000 study of syringe exchange participants in Seattle found that people who participated in a syringe exchange were 2.5 times more likely to reduce their injection frequency than people who had never participated in a syringe exchange program. They were 3.5 times more likely to stop injecting drugs all together (compared to those who had never participated in a syringe exchange program). New users of syringe exchange programs were five times more likely to enter drug treatment programs than those who did not use the programs (13).
Washington state legalized syringe exchange in 1992. Their state health department coordinates the work of many different programs spread around the state. In 2016 87,806 individuals were served, the majority through mobile syringe exchange programs, non-traditional community locations, deliveries, outreach, clinics, and community-based organizations.
In 2016, 16,719,311 sterile syringes were distributed. 5,294 people were referred to drug treatment were made, as were 8,376 health care referrals, and 11,401 people participated in syringe exchange.
Syringe exchange programs are also an excellent opportunity to distribute naloxone and are an extremely effective pathway to prevent overdose deaths. In WA, 2,728 naloxone kits were distributed in the first eight months of 2017. 1,814 people received kits, including 349 law enforcement officers and 1,465 people who use drugs. In just eight months, 392 overdose reversals were reported. 100% of reversals were performed by drug users.
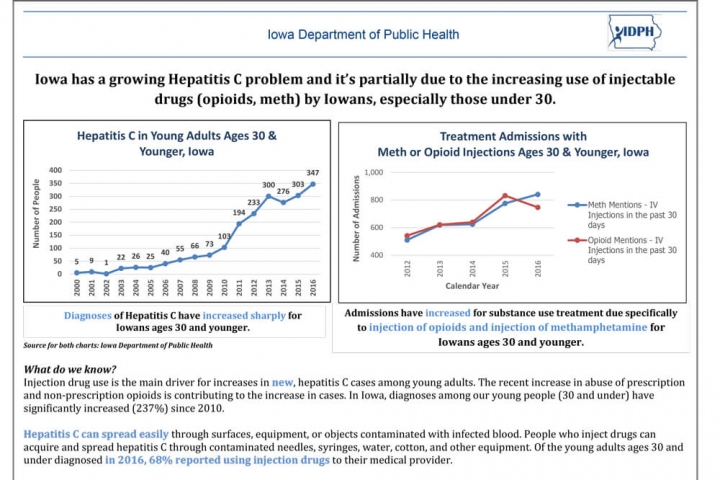
Syringe Service Programs (SSPs) in Iowa
What Law Enforcement, Public Health, & Community Leaders Need to Know
Law enforcement officers will not be responsible for determining whether or not individuals who possess drug paraphernalia have obtained the materials through an authorized SSP. Instead, participants in syringe exchange programs will be issued a unique identification number and a participant card. If law enforcement officers encounter an individual in possession of paraphernalia, it is the responsibility of the individual to demonstrate that the paraphernalia was obtained legally through an IDPH authorized SSP by producing their unique identification number and participant card.
Under the proposed legislation for the 2019 session, law enforcement officers will not be held liable for unknowingly charging syringe exchange program participants with paraphernalia possession, if the charge is issued in good faith.

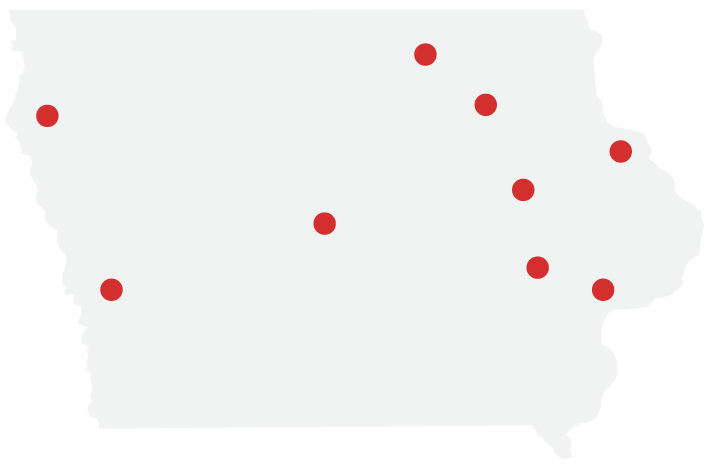
Iowa Department of Public Health (IDPH) will administer the syringe service programs through existing infrastructure for HIV and hepatitis C prevention and care programs. Currently nine programs receive IDPH grants through the Integrated Testing Services (ITS) program. These nine sites will be charged with implementing syringe exchange programs in their communities and the surrounding region, including neighboring counties, small towns, and rural communities.
Programs asked to implement syringe service programs may include:
- Linn County Public Health – Cedar Rapids
- Johnson County Public Health – Iowa City
- Black Hawk County Health Department – Waterloo
- Cerro Gordo County Health Department – Mason City
- Council Bluffs City Health Department – Council Bluffs
- Hillcrest Professional Health Clinic – Dubuque
- Project of Primary Health Care & Polk County Public Health Department – Des Moines
- Scott County Public Health Department – Davenport
- Siouxland Community Health Center – Sioux City
Federal Dollars
In November 2017, the Centers for Disease Control and Prevention approved Iowa to receive federal funding for SSPs, should the state modify the existing drug paraphernalia code. The available funding may be used to pay for program implementation costs, staff time, and program materials. Federal funding may not be used for the purchase of syringes or needles. It is likely that Iowa may receive similar levels of funding to other states with similar geographic distribution and population size. Available funding includes:
HRSA: Up to $500,000
SAMHSA: A portion of the state’s current $2,000,000 State Targeted Opioid Response grant
CDC: Up to $500,000
Private Foundations
A number of private foundations provide annual funding to SSPs around the United States. The Elton John AIDS Foundation is one such major private funder of SSPs in the U.S. and in 2017 provided almost $10 million dollars in grants to SSPs. Dollars from private foundations may be used for the purchase of syringes.
State Dollars
No state funding is requested to support these programs. No funding will be diverted from existing programs. That means no dollars will be taken from law enforcement or substance use prevention program budgets to fund SSPs.
Municipal Dollars
Iowa municipalities will be able to fund the purchase of syringes for SSPs and support other program costs, should they chose to do so.

Sam's story
From 1985 – 1998, Sam used injection drugs. She moved to Seattle from California in 1993, where she began to use a syringe exchange program. At the syringe exchange program, she learned about hepatitis C, and learned not to share syringes or any other injection materials (or even the same space at a table). She shared the knowledge with her friends who she used with.
In 1998, she moved back to her hometown in Minnesota and stopped using drugs. When she returned to Minnesota, she found that everyone she knew and had previously used drugs with had hepatitis C. “No one was hep C free. Everyone I knew had it. And I had stayed away from it.”
Sam credits participating in the syringe exchange as the reason she never contracted hepatitis C. 85% of injection drug users will contract hepatitis C within the first year of use, but HCV can be prevented through safe injection practices. Sam says that she attributes what she knew about hepatitis C “to the folks at the syringe exchange – they knew what to do and what not to do. It was accessible and easy to get to – the convenient access to sterile equipment made it easy not to share materials.”
After Sam returned to Minnesota, she felt like a gift had been given to her in allowing her to survive and stay healthy – she wanted to give back to the community and to other people experiencing addiction. She went to school to be a drug and alcohol counselor, completed an internship at a methadone clinic, and then began to volunteer at the local syringe exchange. She worked at the syringe exchange in various roles for several years before becoming the Executive Director. “I just felt so passionate after being a participant, and by the time I was in a different place in my life, I was able to give back to the community (15).”
Syringe Exchange Starts a Conversation